Ministers have launched a review of the role of physician associates in the NHS – amid fears the less qualified medics are acting beyond their purview.
Physician Associates (PAs) are graduates who have undertaken two years of postgraduate training but do not have a medical degree.
They have hit the headlines in recent years following the deaths of people who were treated by associates but did not know it, and where mistakes were made.
Meanwhile LBC found earlier this year that PAs and AAs had been found to have acted illegally in one in eight NHS trusts.
Despite these concerns the government plans to expand the number of PAs in England from 3,500 to 10,000 by 2036/37, and to hire for 2,000 more anaesthesia associate (AA) roles.
Tom Swarbrick and Dr Alison George on the alarming expansion of physician associates in the NHS
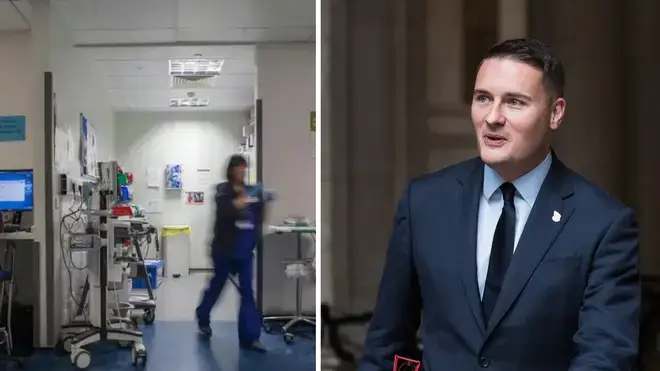
In September the Academy of Medical Royal Colleges wrote to Health Secretary Wes Streeting calling for a review of PAs and AAs amid "mounting concern" from doctors about the roles.
The academy called on the Government and NHS England to look at whether associates are having a negative impact on patient safety, whether they really free up doctors' time for other tasks and whether they improve the overall quality of care for patients.
The Royal College of GPs has also issued its own guidance saying PAs must not see patients who have not been triaged by a GP, and should only undertake work delegated to them by, and agreed with, their GP supervisor.
The review, announced on Wednesday, will be led by Professor Gillian Leng, who is president of the Royal Society of Medicine. She will look at how PAs and AAs affect safety and how they support wider health teams, including GPs.
'It's actually quite offensive, Tom', GP tells Tom Swarbrick
Mr Streeting said: "Many physician associates are providing great care and freeing up doctors to do the things only doctors can do.
"But there are legitimate concerns over transparency for patients, scope of practice, and the substituting of doctors.
"These concerns have been ignored for too long, leading to a toxic debate where physicians feel ignored and PAs feel demoralised.
"This independent review, led by one of the UK's most experienced healthcare leaders, will establish the facts, take the heat out of the issue, and make sure that we get the right people, in the right place, doing the right thing."
Caller Eilidh: “I genuinely think that they're slowly trying to replace doctors…”
The review will examine ways to ensure patients know they are being seen by an associate and the reasons why.
It will also seek evidence from patients, employers within the NHS, professional bodies and academics.
Prof Leng said: "To promote patient safety and strengthen the NHS workforce, it's crucial that we have a comprehensive review of the role of PAs and AAs.
"This will cover recruitment and training, scope of practice, supervision and professional regulation.
"As I conduct this review, I am looking forward to speaking to a broad range of stakeholders and to gathering evidence from the UK and abroad so that we can reach a shared understanding of these roles and their place in wider healthcare teams."
Amanda Pritchard, chief executive of NHS England, said: "Physician associates and anaesthesia associates are important members of NHS staff – they come to work every day to help care for patients and so they deserve to be treated with the same respect as anyone else coming to work in the NHS.
"While we have always been clear that they are not replacements for doctors, there are clear and ongoing concerns which we are listening to carefully and taking action to address – this independent review marks our pledge, together with the Government, to getting this right."
Susan Pollitt's inquest concluded her death at Royal Oldham Hospital in 2023 had been caused by an "unnecessary medical procedure contributed to by neglect".
Meanwhile, Emily Chesterton, 30, died in 2022 from a pulmonary embolism after being misdiagnosed by a PA on two occasions when she visited her GP practice in north London.
She had been under the impression that she was seeing a GP but the PA failed on both occasions to spot her leg pain and breathlessness was a blood clot, which ultimately travelled to her lungs.
A coroner later ruled she "should have been immediately referred to a hospital emergency unit" where she would likely have been treated for pulmonary embolism and would have survived.